The overlooked impact of late Pulmonary Arterial Hypertension (PAH) diagnoses
June 23, 2025 • Reading time 3 minutes
Unexplained breathlessness remains a complex challenge within the healthcare system, often resulting in delayed or incorrect diagnoses of serious underlying conditions. One such condition is pulmonary arterial hypertension (PAH), a rare and progressive subtype of pulmonary hypertension (PH), which is frequently overlooked due to its non-specific symptoms. PAH is characterised by fatigue, chest pain, and breathlessness, symptoms that are frequently present in other conditions. With fewer than 5,000 cases in the UK, the combination of PAH’s rarity and broad symptoms often results in the condition going undetected for years, leading to delays in treatment and worse patient outcomes.
For many patients, the path to diagnosis involves a prolonged and frustrating cycle of investigations, over the course of two or more years. During this time, patients may undergo many different diagnostic tests and make repeated visits to GPs and hospitals, with nearly half initially receiving a misdiagnosis (Small et al., 2024). As the disease progresses, patients find it difficult to do any activities that require physical exertion, including working, climbing stairs, or carrying groceries. It is therefore unsurprising that patients experience a mounting physical, emotional, and financial burden. At the same time, the ongoing cycle of tests and medical consultations places a significant strain on the healthcare system. Early detection and accurate diagnosis are therefore critical to improve patient outcomes and reduce pressure on healthcare services.
What we did
We conducted a socioeconomic and health evaluation of early versus late diagnosis of PAH for Merck Sharp & Dohme (MSD). We outlined the current treatment pathway and constructed a record of the number and type of tests that patients typically undergo from symptom onset to diagnosis. It then became possible to model the costs of the diagnostic cycle that patients often find themselves in. To assess the socioeconomic impact, we also examined employment rates before and after diagnosis, as unemployment is common due to the severity of PAH symptoms (Armstrong et al., 2019). The vast majority of patients (91%) are classified as high severity when diagnosed (Hoeper et al., 2013). Since earlier diagnosis leads to better disease management and slower progression (Galiè et al., 2015), patients may be able to remain employed for a longer period of time. This allowed us to compare the benefits of earlier diagnosis compared to late.
What we found
Early diagnosis was associated with significant benefit, mainly driven by:
- Avoided diagnostic tests;
- Avoided GP attendances;
- Avoided emergency attendances;
- Avoided treatments of misdiagnosed conditions;
- Improved quality of life (measured by QALYs);
- Continued employment post-diagnosis due to receiving appropriate treatment during a less severe stage of the disease.
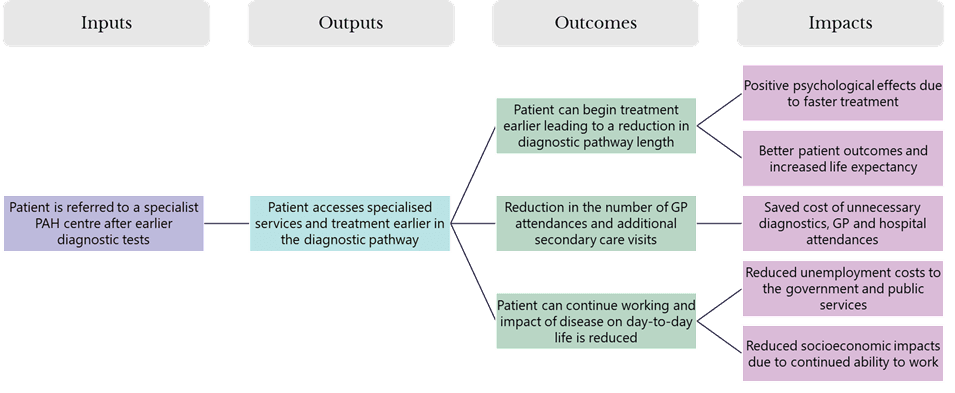
However, earlier diagnosis was also associated with higher costs. These were mainly driven by longer treatment durations, as patients begin therapy sooner and remain on it for longer. Additional costs were also incurred through expanded screening efforts, as increased awareness of PAH may lead to more referrals to specialist services, even for patients who are ultimately not diagnosed with the condition. Nevertheless, the analysis yielded a benefit-cost ratio of 2.0, indicating that for every £1 invested in earlier diagnosis, an estimated £2 is returned. An earlier diagnosis can therefore be regarded as a cost-effective and impactful strategy to improve patient outcomes and generate significant socioeconomic value.
For more details, please see the published image on MSD’s website.
References
Armstrong, I., Billings, C., Kiely, D. G., Yorke, J., Harries, C., Clayton, S., & Gin-Sing, W. (2019). The patient experience of pulmonary hypertension: a large cross-sectional study of UK patients. BMC pulmonary medicine, 19, 1-9.
Galiè, N., Barberà, J. A., Frost, A. E., Ghofrani, H. A., Hoeper, M. M., McLaughlin, V. V., … & Rubin, L. J. (2015). Initial use of ambrisentan plus tadalafil in pulmonary arterial hypertension. New England Journal of Medicine, 373(9), 834-844.
Hoeper, M. M., Huscher, D., Ghofrani, H. A., Delcroix, M., Distler, O., Schweiger, C., … & Pittrow, D. (2013). Elderly patients diagnosed with idiopathic pulmonary arterial hypertension: results from the COMPERA registry. International journal of cardiology, 168(2), 871-880.
Small, M., Perchenet, L., Bennett, A., & Linder, J. (2024). The diagnostic journey of pulmonary arterial hypertension patients: results from a multinational real-world survey. Therapeutic Advances in Respiratory Disease, 18, 17534666231218886.
 Back to News & Insights
Back to News & Insights