Population Health Management Tools in Practice: An Integrated Neighbourhood Teams Case Study
September 4, 2025 • Reading time 4 minutes
The recently published NHS 10-year plan pushes hard on neighbourhood health. Our teams have been working on the ground with teams implementing new neighbourhood health pilots to support the successful delivery of this key NHS objective.
Working with the Population Health Team from Lewisham and Greenwich NHS Trust we:
- Modelled the benefits of their novel Integrated Neighbourhood Teams pathway, expected to go live in 2025, which showed savings of £612,024 (or 342 inpatient bed days and 664 ED attendances avoided) across LGT alone within the first year.
- We defined the core functionality of an effective population health management tool to unlock these savings. This included population level risk stratification and long term benefit tracking.
“Edge provided exceptional support in shaping the INT model and developing clear platform requirements. For the INT work, they delivered a comprehensive framework that could be applied to any project, alongside clear and accessible financial modelling and forecasting of benefits. This approach really accelerated and strengthened our work.
For the platform requirements, Edge helped us create a clear overview of all the essential data and tool components for PHM, enabling us to assess future platform options with confidence.“
Rachael Smith
Population Health Associate Director, Lewisham Health & Care Partners
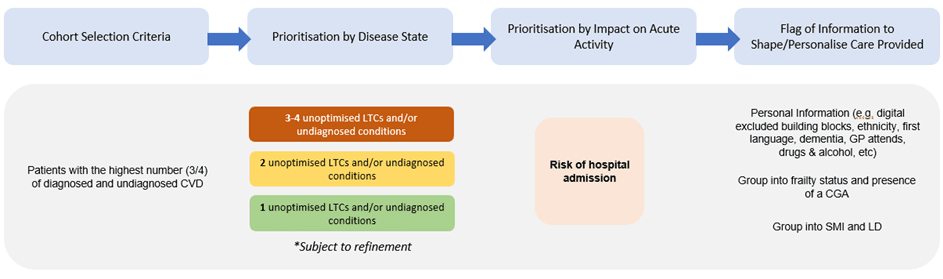
Integrated Neighbourhood Teams in Lewisham and Greenwich: The Pilot Design
Lewisham and Greenwich NHS Trust (LGT) have been ahead of the curve in the design and set-up of Integrated Neighbourhood Teams (INT), with their novel pilot expected to go live in 2025. A key aspect of their approach is the utilisation of their population health management tool, HealtheIntent. The LGT Population Health Team use the tool, which brings together key population health datasets, to proactively risk-stratify patients and identify those with the greatest need. The diagram below shows how these individuals were identified for the pilot.
Identified patients will then be invited to be part of the pilot. Those who agree will be provided a holistic assessment and multimorbidity review which will inform the design of a tailored ~12-week intervention which could include:
- Caseworker provision: single point-of-contact who meets with patient, flags issues, and acts as a point of contact for the team.
- Lifestyle medicine: tailored diet and exercise advice prescribed by INT team to support patient in the community.
- Medicine management: clinical prescribers review, adjust, and deliver new medication plans.
- Group consultations and 1 on 1 support: small workshops and 1-to-1 appointments are conducted to promote adherence and support in the community.
Integrated Neighbourhood Teams in Lewisham and Greenwich: Our Benefit Modelling Support
Edge Health were commissioned to support the prospective benefits modelling for the INT pilot.
Our team started by developing an impact pathway, mapping inputs, e.g. holistic assessment, through to impacts, e.g. reduced general emergency attendances at University Hospitals Lewisham (UHL).
Key to this impact pathway was identifying the beneficiary for each of the identified impacts. In LGT’s model of INT delivery this was particularly important as a key identified benefit is reduced cardiovascular risk, namely heart attacks and strokes. However, UHL does not provide specialist heart attack and stroke services, with patients instead being sent to Guy’s and St Thomas’ NHS Foundation Trust (GSTT) and King’s College Hospital NHS Foundation Trust (King’s) for treatment. Therefore, our impact pathway delineated where benefits would be realised, separating out UHL and wider system benefits.
Our team then used this impact pathway to quantify key anticipated impacts of the pilot. Using validated assumptions, we quantified the impact of the INT to savings to UHL through saved ED attendances and ED admissions. In Year 1 of the pilot, the saving totalled £612,024 (or 342 inpatient bed days and 664 ED attendances avoided).
We also quantified the wider system benefits of the INT by including modelling of savings to GSTT and King’s through avoided STEMI, heart attacks and stroke. Instead of quantifying Year 1 benefits, we modelled out to 10 years post intervention, reflecting the longer-term impacts of the intervention on STEMI heart attack and stroke avoidance. Our modelling found total 10-year savings of £392,819 (or ~13 STEMI heart attacks and ~48 strokes avoided).
Our modelling has since been used to support the business case of the INT Programme within LGT.
The Importance of Population Health Management Tools in the success of INTs
We have shown that INTs can release significant benefits, but the realisation and tracking of these benefits is heavily dependent on population health management tools.
For example, one of the core enablers of full realisation of our modelled benefits in Lewisham and Greenwich is getting this support to the right people. Key to this is risk stratification of the population to identify those most in need. To do this effectively and at scale, population health management tools are essential.
Additionally, population health management tools should enable Trusts to effectively track the progress and benefit realisation of pilots, including for INTs. This enables pilots to adapt early if components of pilot design are not delivering maximum benefits to the population and health system. This should, therefore, reduce wasted resources and maximise return on investment.
However, population health management tools must have the right functionality to support organisations deliver value for money. Our expert data engineers worked with LGT to understand their core functional requirements and what future functionality which could support their population and neighbourhood health aims.
The diagram below provides a high-level summary of the core requirements of an effective tool, considering the full lifecycle from data ingestion and storage to processing, consumption, interoperability, and end-user visualisation. Further details based on the specific requirements within LGT and the population health team were provided to the team.
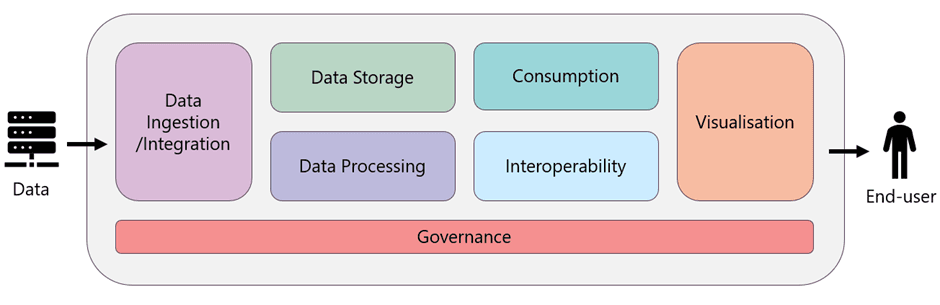
This support will enable the LGT Population Health Team to make important decisions on the future of their population health management tool, including its design, development, and implementation strategy to maximise the tool’s effectiveness and deliver maximum benefits to the population it serves.
 Back to News & Insights
Back to News & Insights

