Evaluation of Proactive Virtual Care for Complex and Chronic Disease Management
December 16, 2025 • Reading time 3 minutes
The growing challenge of complex and chronic disease management in the NHS
Complex and chronic diseases pose a significant and escalating challenge for both patients and the NHS. In England, one in four adults lives with at least two long-term conditions.1 These conditions account for over half of all GP consultations and 70% of inpatient bed days.2 The challenge is particularly acute in Leicester, Leicestershire, and Rutland (LLR) ICB, where an older population and significant deprivation add further complexity to the risk of chronic illness.
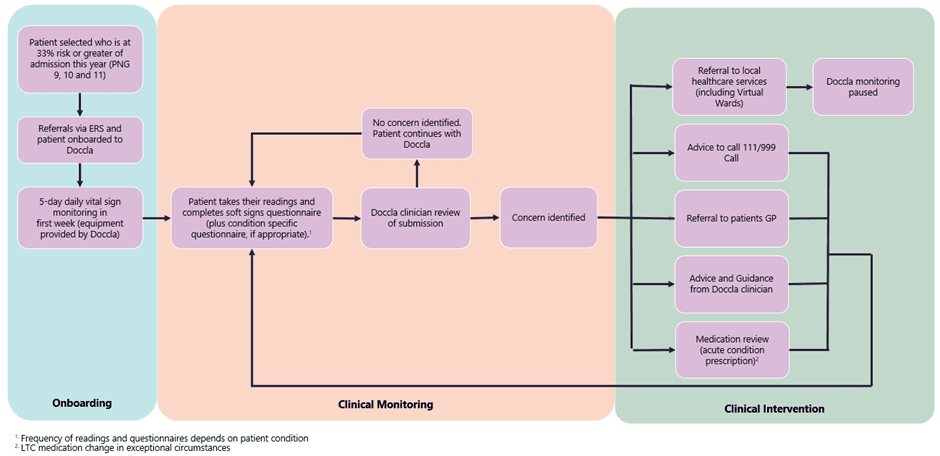
The LLR-Doccla Virtual Care Programme was launched to address these challenges by providing proactive detection of patient deterioration. It was specifically designed for patients in Patient Needs Groups (PNGs) 9, 10, and 11; the most complex and multi-condition needs groups who also had a 33% or greater risk of hospital admission.
During a nine-month pilot, 56 successfully onboarded patients received remote monitoring, including virtual vital sign monitoring (such as a smart device, blood pressure cuff, and thermometer) and soft signs questionnaires. When Doccla clinicians identified concerns (a “red alert,” which occurred in 59% of over 4,500 completed questionnaires), they intervened with a consultation (1,200 total) or escalated the patient to the appropriate services, like their GP, a local healthcare service, or emergency services.
Our Approach: Impact and Economic Evaluation
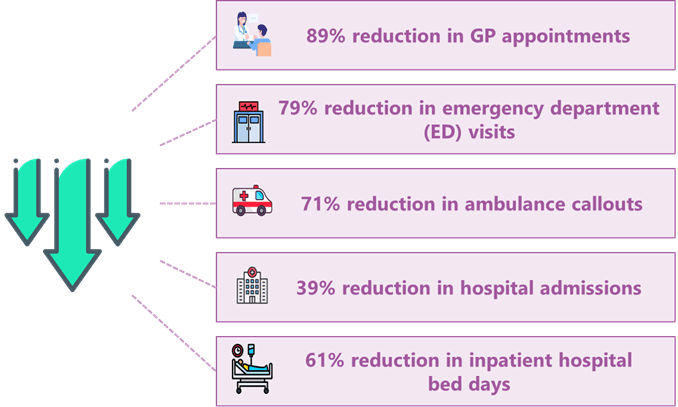
The evaluation quantified the programme’s impact by comparing the healthcare utilisation of pilot patients to their estimated pre-pilot usage (the counterfactual, based on local and national data). This comparison showed significant reductions in healthcare usage, with estimated reductions scaled to a full nine-month period:
- GP appointments reduced by 89% (337 appointments avoided).
- Emergency Department (ED) visits reduced by 79% (33 attendances avoided).
- Ambulance callouts reduced by 71% (5 callouts avoided).
- Hospital admissions reduced by 39% (30 admissions avoided).
- Inpatient hospital bed days were reduced by an estimated 61% (227 days reduced on average).
We also conducted patient survey which revealed a largely positive experience, with 95% of respondents rating the service as “Good” or “Very Good.” Patients particularly valued the quick access to care and the reassurance of having their health monitored. Over 60% of respondents reported feeling safer and more in control of their health, with the service contributing to an improved quality of life.
What We Found
The overall reductions in healthcare utilisation led to estimated capacity-releasing savings of more than £160,000 over the nine-month pilot.
Comparably, the total cost of the pilot was £274,000, generating a pilot cost-benefit ratio of 0.6. This means that for every £1 spent, the healthcare system only saw a return of 60 pence. Exploration of this lower-than-expected return on investment found low patient recruitment compared to target levels (56 patients recruited versus a target of 185), due to coinciding GP collective action, contributed. A sensitivity analysis found that if the pilot had successfully recruited its full target of 185 patients for the full pilot duration, the estimated benefits would have resulted in a significantly favourable cost-benefit ratio of 1.96.
Although the LLR ICB team made efforts to simplify the recruitment process to lessen the burden on GP practices, its impact was not seen due to the pilot’s short time frame. Nevertheless, the pilot demonstrated system wide benefits with a small sample of patients for LLR, and we are now considering how we model this way of working in our future Neighbourhood plans.
In conclusion, proactive virtual care can be a helpful tool in managing the rising tide of chronic conditions, with the potential to deliver financial benefits, reduce avoidable healthcare utilisation, and improve patient experience. However, our report highlights that managing the risks of low recruitment (e.g. recruitment-variable contracting) due to the widespread pressures on the NHS are important to maximise return on investment.
“Edge Health were our evaluation partners for the pilot, and they joined right at the initiation of the project and were able to offer advice and support for our evaluation and Information Governance requirements. Edge Health came with us on our journey to design and implement and were always a valuable part of the project team. Edge Health were always professional, patient, and responsive to our needs and working with Lucy, Izaak and Aditi has been an absolute pleasure. I would highly recommend Edge Health as evaluation partners and very much look forward to working with them again in the future.”
Tracey Knight
Senior Integration and Transformation Manager, LLR ICB
 Back to News & Insights
Back to News & Insights


